Useful information for doctors and those treating patients
Things to know for practitioners
Where can I find further regional treatment offers for Long COVID patients?
You will find a range of clinics with a specialisation for Long COVID in the Service area, where you can search for offers in your neighbourhood for your patients.
Last update: June 2023
Where can doctors find more information on treatment of patients?
Guidelines, consensus papers
The S1 guideline Long/Post-COVID offers detailed information on diagnostics and treatment of Long COVID patients. The guideline also illuminates on the aspects of rehabilitation. It is what is called a living guideline, which is reviewed and updated annually. It was created in an interdisciplinary collaboration by multiple medical societies. The corresponding Patient guideline Long/Post-COVID syndrome can be issued as a information leaflet to long haulers and their relatives, loved ones and caregivers.
In November 2021, NICE, the National Institute for Health and Care Excellence in Great Britain published a revised guideline (Rapid Guideline) with recommendations for diagnosis, treatment, and multidisciplinary rehabilitation of Long COVID in adults, children, and adolescents.
A Consensus paper was formulated in May 2022 for the standard basic care of children and adolescents in collaboration with multiple societies of paediatricians. The paper combines the current expert opinions on various clinical aspects of Long COVID in children and adolescents and states the treatment recommendations. An S2k guideline for diagnosis and therapy of Long COVID in childhood and adolescence is already registered and shall be published in 2025.
The Deutsche Gesellschaft für Neurorehabilitation e. V. [German Society for Neuro-rehabilitation] (DGNR) has issued an S2k guideline COVID-19 and (Early-)Rehabilitation, which looks at aspects of rehabilitation in Long COVID patients.
The S2k guideline on Neurological Manifestations in COVID-19, which was issued by the German Society for Neurology (DGN), is specifically pursuing the treatment options for symptoms of the nervous system. This guideline also discusses the possibilities of neurological rehabilitation.
With regard to myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS), a Consensus statement for diagnosis and treatment of ME/CFS was published in May 2024. This publication summarises the current state of knowledge on ME/CFS including the diagnosis and current treatment options.
The S3 guideline Tiredness by the German Society for General Medicine and Family Medicine (DEGAM) also contains information on ME/CFS in Chapter 5.7. The guideline is also available as a patient guideline.
There is a S2e Guideline of the Deutsche Gesellschaft für Neurorehabilitation e.V. (DGNR) regarding the Post Intensive Care Syndrome (PICS). Apart from that, a corresponding Patient guideline is available. It addresses patients who were treated or given artificial respiration at the intensive care unit for a long time.
Therapy compass for symptom-oriented drug therapy
The external group on Long COVID Off-Label-Use at the Federal Institute for Drugs and Medical Devices (BfArM) has developed a therapy compass, which offers an overview of the suitable active ingredients and active ingredient groups with the aim of supporting care of patients with Long COVID and giving practical recommendations for medical treatment.
These prescription drugs are prescribed as a part of their existing approval, so, as in-label-use. These are expert recommendations for a symptom-oriented treatment, based on the current guidelines and German context of patient care. The therapy compass contains concrete examples within certain substance classes based on the experiences of expert groups. The compass contains drug therapy recommendations for a total of 12 symptoms typical to Long COVID. It also gives information on dosing. The drugs can be prescribed on the basis of the symptoms in the context of their existing approval (“In-Label-Use”). The costs for the drug therapy are therefore borne by the statutory health insurance company as a rule. The therapy compass is made available on the Website of BfArM.
Advanced multimedia training
Moreover, there are advanced trainings, which aid knowledge sharing on Long COVID in the medical circles. In this way, the Post-COVID Network of the Charité – Universitätsmedizin Berlin offers a regular advanced training series on Long COVID. Every advanced training course consists of the presentation by an expert and a subsequent case study with all the participants. Interested parties also have the option to propose a case presentation at the time of registration. The records of previous events can be viewed in the archive. You can find more recommendations for advanced training on the website of Post-COVID Network of the Charité.
The presentations from the 1st Congress of the Doctor’s Association on Long COVID from November 2022 were also recorded and are freely available.
Further information can also be found at the Robert Koch Institute. It provides scientifically substantiated information on Long COVID on its info portal. Recommended literature of scientific publications in English are also available in our Service section.
Long COVID guidelines of the Joint Federal Committee
For a quick and need-based care of patients with suspicion of Long COVID, a new Guideline of the Joint Federal Committee (G-BA) has become operative on 9 May 2024. This Long COVID guideline defines the requirements for care and describes the so-called care path, i.e., the course of medical treatment.
A medical contact person is appointed. They shall undertake the necessary specific coordination in diagnosis and therapy. Thus, the existing outpatient structures and programmes are used need-based depending on the severity and complexity of the illness and the right healthcare professions are involved.
Overview of guidelines and training courses:
Guidelines, consensus papers
Patient guideline Long/Post COVID Syndrome
NICE: COVID-19 rapid guideline: managing the long-term effects of COVID-19
Consensus paper Standard basic cared of children and adolescents with Long COVID
S2k guideline COVID-19 and (Early-)Rehabilitation
S2k guideline Neurological Manifestations in COVID-19
S3 Guideline Tiredness by the German Society for General Medicine and Family Medicine (DEGAM)
S2e Guideline Multimodal Neuro-rehabilitation Concepts for Post-Intensive Care Syndrome (PICS)
Therapy compass
Long COVID Expert Group on Off-Label-Use
Advanced multimedia training
Records of the events of Post COVID network of the Charité – Universitätsmedizin Berlin
Records of presentations from the 1st Congress of the Doctor’s Association on Long COVID
Also consider our information specifically for employees and employers. Under the heading “Things to know about Long COVID in professional context”, you will find information and points of contact on topics such as Long COVID as accident at work, loss of profession due to Long COVID, Long COVID in work routine and going back to work.
Long COVID guidelines of the Joint Federal Committee
Last update: December 2024
What are the options for the treatment of Long COVID?
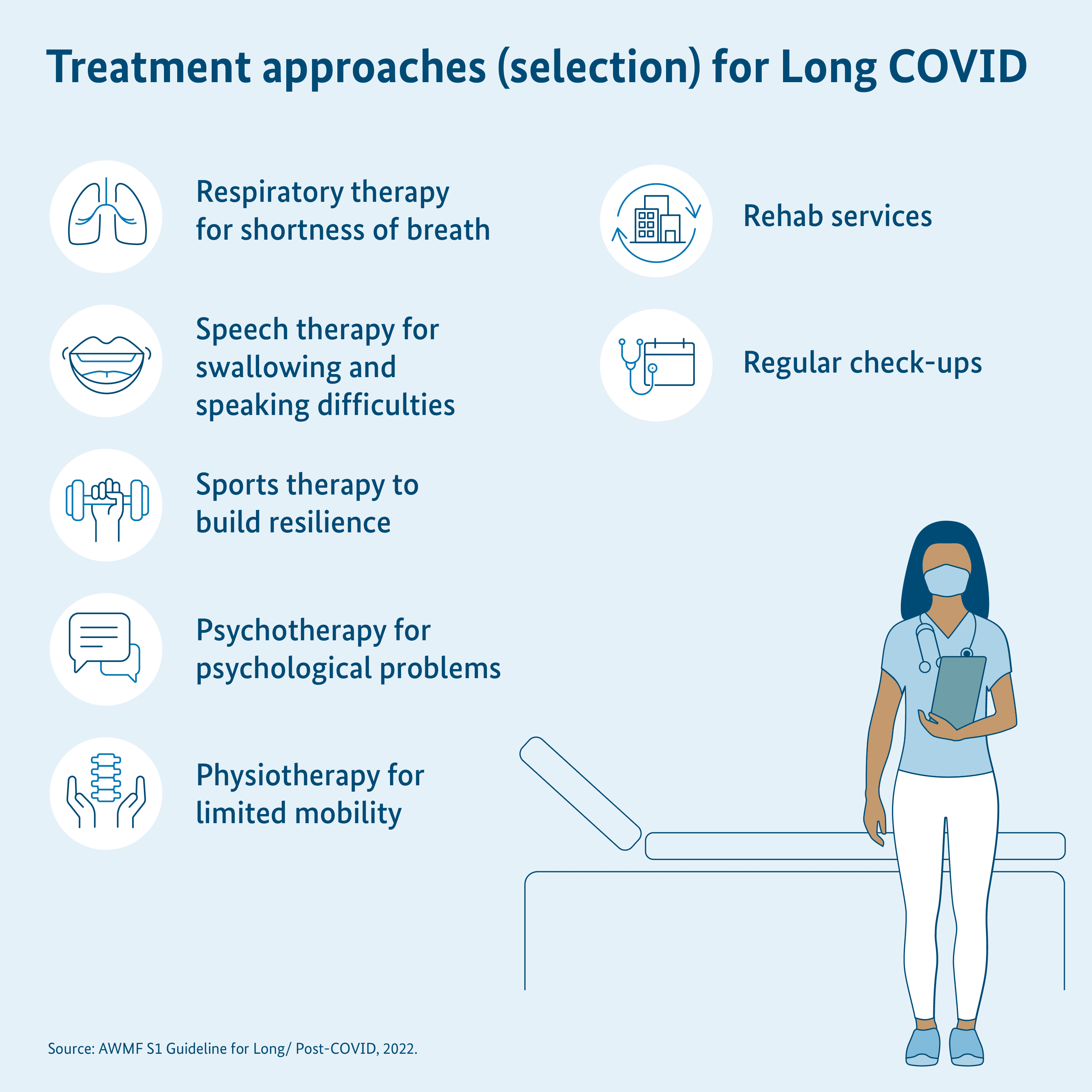
There is no uniform treatment of Long COVID as yet. Among other things, this is due to the fact that the illness can be accompanied with many different symptoms. These symptoms can resemble one another in part. However, their progression and characteristic can greatly differ individually. Different healing professions have to collaborate to adequately treat Long COVID. Continuous care is necessary and the collaboration of various medical disciplines is needed for this purpose.
There have been no treatments until now, which counter the disease development (“causal therapy”). The treatment concepts until now aimed at alleviating the symptoms (“symptomatic therapy”). In many cases, the symptoms become weaker or disappear on their own over time. In other cases, they change, return or even become stronger. An early treatment can be helpful to avoid the development of long lasting symptoms. This is especially true for patients with a deterioration of the symptoms following an activity (so-called “stress intolerance”).
The family doctor’s practice is the first point of contact for long haulers. The family doctor either treats the long haulers himself or refers them to a specialist practice. At present, various treatment approaches are used in Long COVID. These include:
- a breathing therapy, for example, for treating shortness of breath,
- a logaoedic treatment, which can be helpful in dealing with problems in swallowing and speech,
- a sports therapy to train capacity and rebuild physical endurance (Attention: In case of a stress intolerance, the symptoms can become intensified by physical activity. In this context, also read the question “Are there scientific insights on the treatment of ME/CFS?”. If the daily routine activity has declined due to stress intolerance, pacing can be a helpful strategy: “What is pacing?)
- a physiotherapy or remedial gymnastics, which is useful in severely limited mobility,
- ergotheray (e.g. stress training or brain performance training),
- a psychotherapeutic or supplementary psychiatric treatment, which can support in psychological problems,
- a nutrition therapy, for example, in case of food intolerances or severe weight loss,
- intake of specific medicinal products,
- regular check-ups to monitor the symptoms over time and adapt the treatment methods,
- various rehab offers for long haulers.
Medications can also be used depending on the symptoms. These can help, for example, in alleviating severe circulatory disorders or sleep disturbances. In principle, the respective doctor shall agree upon the treatment options together with the patient. While doing so, healthcare professionals should always take into consideration the latest medical knowledge and obligation of medical due diligence. The treatment should also be done according to prudent discretion. Information on the treatment options are given in the S1 guideline Long/Post COVID. The Consensus Statement for Diagnostics and Treatment of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome also has orienting treatment suggestions for which there is only weak scientific evidence of their effectiveness.
The treatment options for circulatory disorders (orthostatic hypotension, postural tachycardia syndrome) are described in the S1 Guideline “Syncope” of the German Society for Neurology.
Overall, further research is still needed to understand the exact cause of Long COVID and find out which treatments and medications are effective. Until then, the goal is to alleviate the individual symptoms.
Last update: December 2024
Where can doctors find more information on administrative questions regarding Long COVID diagnostics and treatment?
Post COVID (U09.9) is nationally recognised as a special prescription requirement in provision of remedies. This means that medically necessary physiotherapy or ergo-therapy can be prescribed by the attending doctor without the resulting prescription costs straining the practice’s budget. The required remedy can be prescribed for a period of 12 weeks depending on the prescription. The same applies for psychological symptoms due to long-term effects of Corona infection; a prescription can also be issued by the affiliated psychotherapists here. The National Association of Statutory Health Insurance Physicians (KBV) provides information on the performance audit and billing of diagnostics and therapy of Long COVID as well as administrative procedure.
The KBV has provided a common diagnosis list for long-term remedy and special prescription requirements on its website:
https://www.kbv.de/media/sp/Heilmittel_Diagnoseliste_Webversion.pdf
Last update: June 2023
What is the role of psychosomatic aspects in Long COVID?
Researchers largely agree that Long COVID is not an illness of psychological cause. According to the current state of knowledge, various mechanisms are involved in the development of Long COVID. These include persistent inflammatory reactions, a dysregulated immune and autonomous nervous system, viruses or viral components remaining in the body and an impaired mitochondrial energy metabolism.
The extent to which psychosomatic aspects play a role in the development and preservation of Long COVID is not sufficiently clear. Psychosomatic interactions are interactions between the mind and the body. Psychological symptoms can lead to physical illnesses or favor them. For example, current or earlier stress factors can have an impact on the body. But your own personality, expectations as well as psychological illnesses such as depression or anxiety disorders can also have an effect on physical symptoms. It is a challenge in Long COVID also to gauge the interactions between physical and psychological processes.
An article from the journal Psychosomatic Medicine in the April 2021 issue describes how psychological, social, and cultural factors as well as environmental influences can influence the progression of a COVID-19 illness. The article underlines the importance to regard the illness not just purely biologically, but also consider other factors.
It is most important for medical practice to take the symptoms of long haulers seriously. It applies here to regard the patients from all points of views and treat them accordingly. Just like in other chronic illnesses, it is important to consider not only the biological aspects, but also the psychological and social aspects. Independent of the causes of illness, psychotherapy can have a positive impact on coping with Long COVID and its progression.
Sources:
https://www.nature.com/articles/s41579-022-00846-2
https://www.bmj.com/content/374/bmj.n1648
https://linkinghub.elsevier.com/retrieve/pii/S1473309924002111
https://www.nature.com/articles/s41467-023-44432-3
https://www.nature.com/articles/s41380-022-01836-9
https://www.mdpi.com/1648-9144/59/4/719
Further information:
https://register.awmf.org/de/leitlinien/detail/020-027
Last update: June 2023
What is the focus of the current research on Long COVID and ME/CFS?
Long COVID has been the subject of intensive research for as long as the illness has been known. The clinical pattern of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome (ME/CFS) has also come more into focus of research since then.
The important focus points of the German and international research on Long COVID are currently on the following areas.
- potential risk and protection factors (prevention)
- The spread of Long COVID as well as specially affected population groups (epidemiology)
- individual and social impacts of Long COVID on the quality of life, functionality, incapacity of work, and healthcare requirements (healthcare research)
- Detection of a clinical pattern, causes of the disease and disease progression (pathogenesis)
- Indications and health problems (symptoms)
- Options for assessment of Long COVID (diagnostics)
- Options of therapeutic technique (clinical research on therapy options and rehabilitation research)
The Robert Koch Institute (RKI) in its Frequently Asked Questions provides information of the current research projects among other things. You will also find information on the funded projects on the Website of the Federal Ministry of Education and Research (BMBF). An overview of the research in the field of ME/CFS is found in the ME/CFS Research Register.
An overview of the scientific publications until now can be found in our service section. The latest publications are added there every month.
Last update: November 2024
Useful links
Dealing with Long COVID on a day-to-day basis
Communication with others
Information about ME/CFS
- Interdisciplinary, collaborative D-A-CH consensus statement on the diagnosis and treatment of myalgic encephalomyelitis/chronic fatigue syndrome
- Information from the Charité Fatigue Centre on ME/CFS
Information material for downloading and ordering
